Before the cancer I had been a pretty heavy coffee drinker. I drank it not only because I was addicted to the caffeine and the boost it gave me, but also because I really do enjoy the taste of a well-brewed cup o’ joe. A good cup of coffee, just like a good glass of wine, really does [cliche alert!] make life worth living.
Before the cancer I had been a pretty heavy coffee drinker. I drank it not only because I was addicted to the caffeine and the boost it gave me, but also because I really do enjoy the taste of a well-brewed cup o’ joe. A good cup of coffee, just like a good glass of wine, really does [cliche alert!] make life worth living.
I was a late bloomer as a coffee drinker. Though I always loved its smell growing up—I still have vivid, fond memories of the bubbly coffee percolator sounds and the delicious coffee smells that I woke to every morning as a child—I found its taste repulsive and the heated spoiled crap breath that all coffee drinkers blast out even more so. I didn’t want to be complicit in that.
But after high school I joined the navy and, like an idiot, immediately started smoking cigarettes, a habit that previously had disgusted me even more than drinking coffee. If I could force my body to accept and then to crave and then to fervently demand a steady intake of toxic death fumes, then it would stand to reason that hooking myself on coffee couldn’t be too far behind.
Actually, it took another six years.
What finally got me to join the Caffeine Club was the twelve-hour watches that I had to “stand” while stationed aboard my first ship.
I had stood twelve-hours watches all during my time in the navy prior to transferring to the ship, but those watches had always been in large, noisy, bustling communication centers with teams of sailors, which meant that there was always someone around to talk to and to keep me awake during the brutal night shifts. But on the ship, I stood my watches in a quiet, closet of a room by myself and boy could those midnight watches, or mid-watches as the navy jargon goes, get boring.
Thus, in 1989 began my addiction to coffee.
Coffee and Cigarettes. A heavenly match made in hell.
Fortunately, I was able to kick the cigarette habit about a year later.
But I drank coffee like mad until my cancer.
While I initially started drinking coffee as a crutch to get me through the night, I still hated the taste and had to load in piles of cream and sugar to try to cover it up. Over time, however, I eventually acquired a taste for the bean. But my passion for the bean didn’t really come until years later after my father casually remarked that to really enjoy coffee, it needs to be drank black. Unpolluted, so to speak.
So I tried it black. And, like most fathers are, he was right. From then on, I no longer was a man who preferred his coffee “sweet and blond” but one who preferred it “bold and black.”
I drank it that way pretty hard for twenty years.
But when the cancer struck, I had no qualms about quitting. In fact, I didn’t decide to quit, I just did without even realizing it. I guess my subconscious took over after they started pumping me full of chemo and steroids and other crap and spared me of any coffee or wine cravings during my year-long treatment and recovery.
Throughout my years as a coffee drinker prior to cancer, every once in a while I would try to get healthy and ween myself off of caffeine. Not that caffeine is a particularly unhealthy addiction as far as addictions go; but it still is an addiction and deep down, I guess always felt a little uneasy about my dependency on it.
I don’t remember exactly when the last time was I tried to stop consuming caffeine, but I do remember how much it hurt: the eyeball shattering headaches; the total body aches; the nasty moods.
I remember being stuck in traffic for a very long time once during my last attempt at the last weening process and having my legs ache so badly that I thought I was going to have to pull over to the side of the beltway and have the wife come pick me up. I was jonesing bad. I struggled on, but as soon as I got out of traffic I drove directly to the store, bought two cups of coffee, downed one right in the parking lot, and begged forgiveness and mercy from the other one as I lovingly nursed it all the way home.
I probably went through the same kind of withdrawal pain and discomfort when I quit drinking coffee after the cancer diagnosis, but there was already so much other pain and discomfort going on from the blood clots and the treatment that the withdrawal stuff just mixed right in and went unnoticed. Thankfully.
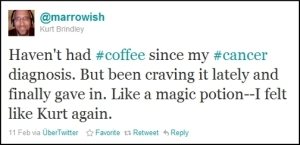
And for over a year during my treatment and recovery process I had no urge whatsoever to start the habit back up. Until recently.
When the urge returned, it returned with a vengeance.
I started drinking it like I never stopped. There was one big difference when I started back up though:
Decaf.
I know, I know. Drinking decaffeinated coffee is like having sex without the climax. What’s the point, right? But, I figured, since I have to take an overload of drugs every day that are already throwing my mental state out of whack, it might be best not to include a stimulant like caffeine into the mix.
So it was decaf for the first couple of weeks.
Until the first time I ran out of it and mistakenly bought a bag of the real stuff.
Why would Starbucks make the bag green if it wasn’t for a decaffeinated coffee?
One good thing about drinking decaf coffee is that I can drink it in the evenings without having to worry about it cranking me up for an all-nighter.
I made the first cup from the mistaken identity bag around 7:00 pm. I think I finally fell asleep around 6:00 am the next day. By 2:00 pm, I was back at the store buying real decaf this time, which was not packaged in a green-themed bag, by the way.
What’s up with Starbucks thinking they can set their own standards?
I have always been very sensitive to drugs and other foreign substances. For instance, it’s hard for me to use morphine or codeine as pain killers because of this sensitivity (remind me later to write an article about my first experience with morphine…ugh).
Even caffeine in the smallest of amounts can overly stimulate me (it’s not often I get to say that out loud) to the point of annoyance to anyone who happens to be around me.
My daily cocktail of drugs are no exception to this sensitivity rule.

The biggest culprit from the cocktail mix for jerking me around is the prednisone. Prednisone is the drug of choice, in fact, it’s just about the only choice, to treat Graft Versus Host-related diseases, of which I am suffering from, and for which I am taking the prednisone.
It addition to GVHD, prednisone is also regularly prescribed for many inflammatory-related illnesses, like asthma or COPD. Because of its potency, it is usually prescribed in low doses, around 5 – 10 mg, for short periods of time, around 7 – 10 days, or so.
Well, I started at 200 mg and now I’m down to 60 mg. I’m going on my fourth month and, even though the treatment doesn’t seem to be slowing the advancement of my lung disease, unless there is a new miracle discovery, I will probably will be taking high doses of prednisone for the rest of my life.
Speaking of miracle discoveries, I will be participating in an NIH study in April 2011 for a new Lung GVHD treatment—fingers crossed.
It kind of freaks me out whenever I visit with a new doctor and their eyes widen and mouths drop when they hear that I’m taking 60 mg of prednisone every day.
The reason they react the way they do is because prednisone has a slew of annoying side effects and is one of those drugs where the cure could turn out to worse than the disease. It causes bone density loss, diabetes, sodium retention, water retention, insomnia, moon face (for some reason it makes the body fat accumulate around the face—my head is friggin’ ginormous!), and worst of all, anxiety, depression, and mood swings.
What fun.
Because of my sensitivity to drugs, I seem to be really affected by the anxiety, depression, and mood swings.
You might be thinking, like I would be if it wasn’t me who was the one saying it: Brindley, get over it. It’s all just in your head.
And my response would be: You’re exactly right! That’s what makes it even worse. I do know that it is all just in my head. But I’ll be damned if I can get it out.
The more I can keep my mind actively engaged, the better off I am.
This blog is great therapy.
So are naps.
But sometimes my mind gets stuck in a deep rutted ravine filled with all of my fears and doubts and I can’t get out no matter how hard I try. It really is crazy because even as I am trapped in this dark place, I know that a big reason why I’m there is because of a drug that is supposed to be saving my life.
And once I get stuck there I usually can’t get out until the drug wears off, which is about twelve hours after taking it.
So, the next time I ran out decaf and decided to go to the real stuff, I had to take all of this into consideration. I knew there could be consequences from the caffeine so, to try to make good out of my stupidity for willingly hooking myself back onto something I had not needed for over a year, I had decided to treat it all like an experiment. When drinking caffeinated coffee while taking the prednisone and other drugs, which would be anytime I drink caffeinated coffee, I would pay close attention to how they interact and affect me.
Good idea, right? 😉
What I found is interesting and somewhat promising.
Pros:
- Caffeine, like the true stimulant that it is, seems to balance out the negative effects of the prednisone. By drinking caffeinated coffee in the mornings when the drugs are at their nastiest, I do not seem to be feeling as depressed and grouchy.
- It seems to be easier to breathe when I take my walks. After some research, I found that caffeine is a xanthine derivate. Xanthine is used to help treat asthma. Maybe this explains why it seems that I’m breathing easier on my walks.
- Caffeine is a diuretic. Diuretics make you pee. This is useful for me since I tend to retain water because of the GVHD.
- Because of the prednisone, I also retain sodium. I don’t understand all this diuretic stuff enough but it could be a good thing if caffeine is of the type that flushes out sodium. I’ll have to follow up with the doc on this.
Cons:
- In addition to the depression, prednisone also makes me anxious and edgy, and increases my heart rate. Adding caffeine into the equation only amplifies that feeling.
- Because of my GVHD, I have dry, itchy skin and my mouth gets dry easily. The steroids help, but since caffeine is a diuretic and I’m peeing all the time I get dehydrated quickly, which only exacerbates the dry skin and dry mouth. I have to drink more water to compensate, which means even more peeing. Its a tedious balancing act.
- Again, I don’t understand much about diuretics, but I read that certain types flush out a body’s potassium. This isn’t good because prednisone already tends to decrease potassium levels. Need more info.
- Because of all the meds I’m taking, my liver is really taking a beating. Since caffeine is metabolized in the liver, I really need to be careful here.
So, to make a long story short… What? Oh…yeah, I see. Too late for that. I guess I got to rambling a bit. Thanks for bearing with me.
In conclusion… better? …my long, rocky love affair with coffee has resumed once again and I find that my passion for the drink is as strong and true as its seductive flavor is bold and addictive.
And now, not only do I drink the brew to fulfill my own selfish desires and dependency, I drink it also to fulfill a broader need, one with an utilitarian, more nobler purpose—I drink it in the name of medical research.
Just think, what started out as an aide to help me better defend my country during my navy years (that sounds much better than calling it a crutch to help me stay awake during boring mid-watches), may turn out to be the impetus behind a cure for a very serious mental health condition.
Now, whenever I drink coffee while strung out on prednisone, I may be one cup closer to understanding the longterm synergistic and psychological effects on the brain from simultaneously consuming large quantities of both stimulative and depressive agents over long periods of time.
My research is going to have an extremely significant and beneficial impact on the entire mental health community. Better lives will be lived because of it.
Yeah, that’s all a bunch of BS, I know (see Disclaimer). But hey, if it helps me to rationalize my pathetic, self-induced dependency on something that I probably shouldn’t be messing with in the first place, why not, right?
Have I mentioned how long it’s been since I’ve had a glass of wine?